Hormonal Regulation of Blood Glucose Levels: Explained
 Posted On
Posted On
Contents
- Introduction
- What is anatomy, physiology and function of Pancreas?
- Pancreas shape and size
- Location of Pancreas
- Parts of Pancreas
- Endocrine and exocrine function of Pancreas
- How is digested food absorbed into the blood and converted into glucose?
- How do hormones regulate blood glucose levels?
- Role of Insulin
- Role of Glucagon
- Role of Somatostatin
- How is glucose oxidised to provide energy?
- Do brain cells require Insulin for glucose uptake?
- What is the difference between insulin and glucagon hormone?
- Conclusion
- FAQ
- Q 1. Which gland secretes Insulin and Glucagon?
- Q 2. Which hormone regulate blood sugar level?
- Q 3. What are the hormones secreted by the Pancreas?
- Q 4. What is the main role of Insulin?
Introduction
Have you ever thought about how our body regulates blood glucose levels throughout the day? Today, we will discuss the hormonal regulation of blood glucose levels in the human body.
Suppose you are driving a car and find improper brake and accelerator functioning.
What will happen?
Your car will be imbalanced; you may get an accident. You must have a proper brake and accelerator in your car while driving.
Similarly, our body has a brake and accelerator. Here, Glucagon works as an accelerator, and Insulin act as a brake.
These two key hormones (Insulin and Glucagon) are vital in maintaining blood glucose level (or glucose homeostasis) in your body.
If there is a problem with your Insulin or Glucagon, you may have an imbalance blood glucose level. It may be either a high blood glucose level or a low blood glucose level.
This post will describe the hormonal regulation of blood glucose levels. Moreover, we will see how Insulin and Glucagon work together to maintain homeostatic glucose levels.
Let’s get started.
What is anatomy, physiology and function of Pancreas?
Our blood glucose level is regulated by Insulin and Glucagon hormones. These two hormones are released from Pancreas.
So, let’s first know about Pancreas.
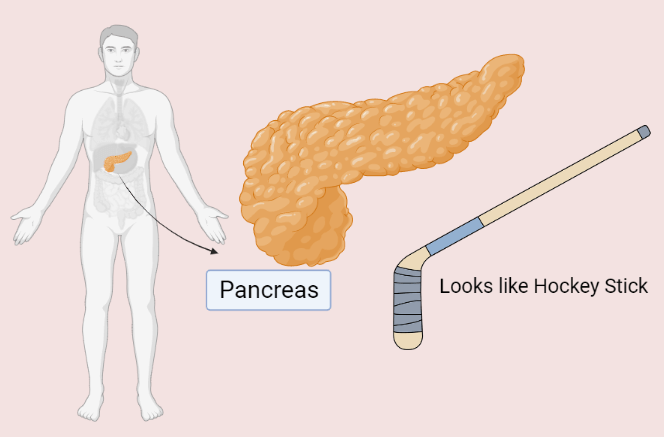
Pancreas shape and size
Pancreas is a J – shaped organ that looks like a hockey stick. The normal size of the Pancreas is about 12–15 cms long, which is just about the length of your hand.
Location of Pancreas
Pancreas is generally located behind the stomach and above the duodenum intestine. It is surrounded by many organs, such as the gallbladder, Liver, stomach, spleen and small intestine.
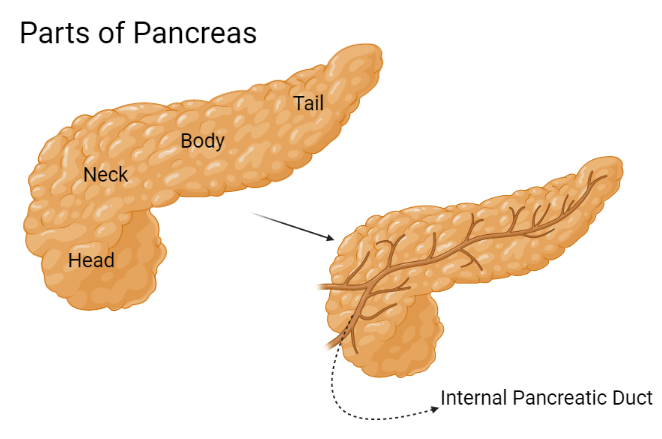
Parts of Pancreas
There are four parts of the Pancreas –
- Head (3 cm) – The widest part of the Pancreas lies in the curve of your duodenum.
- Neck (2.5 cm) – The short part of the Pancreas between the head and body part.
- Body (2.5 cm) – The middle part of the Pancreas between the neck and tail part.
- Tail (2 cm) – The thinnest part of the Pancreas on the left side of the abdomen, located near your spleen.
Endocrine and exocrine function of Pancreas
Pancreas is one organ, but it has two different functions –
- Help in digestion, and
- Maintain blood sugar level
Our Pancreas also acts as a gland that works as an endocrine and exocrine gland.
This exocrine gland contains acinar cells that help in digestion. In contrast, the endocrine gland has an Islet of Langerhans that maintains blood glucose levels.
Let me explain in Nutshell –
Pancreas contains two important cells – Acinar cells and an Islet of Langerhans.
Acinar cells have an exocrine function, which is present nearby the internal pancreatic duct. These cells secret key digestive enzymes (like pancreatic amylase, protease and lipase) and drain into your pancreatic and bile duct, eventually reaching the small intestine. These digestive enzymes help digestion and metabolism of your food like carbohydrates, fat and protein.
On the contrary, the Islet of Langerhans is a cluster of cells that are scattered within the Pancreas but more abundant at the tail of the Pancreas. Around more than 1 million islets of Langerhans are present in your Pancreas.
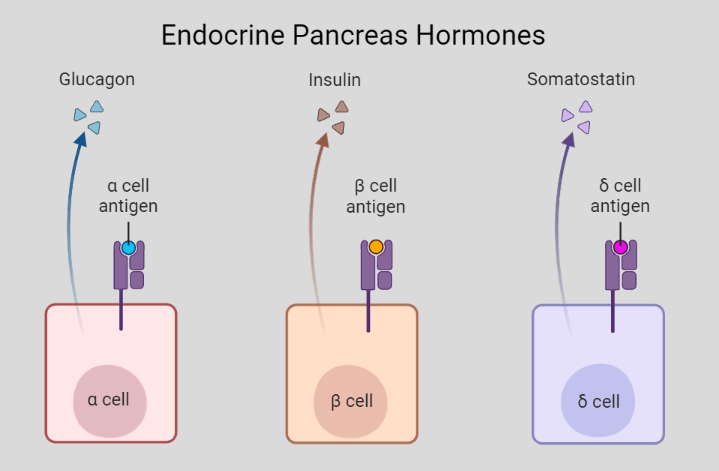
These islets of Langerhans cells have an endocrine function and secrete some peptide hormones from different cells like –
- Insulin from beta cells
- Glucagon from alpha cells
- Somatostatin from delta cells
- Pancreatic polypeptide from F cells
These peptide hormones are secreted in your bloodstream and regulate blood glucose levels. Among these, Insulin and Glucagon are crucial hormones of the Pancreas that manage your blood glucose level.

How is digested food absorbed into the blood and converted into glucose?
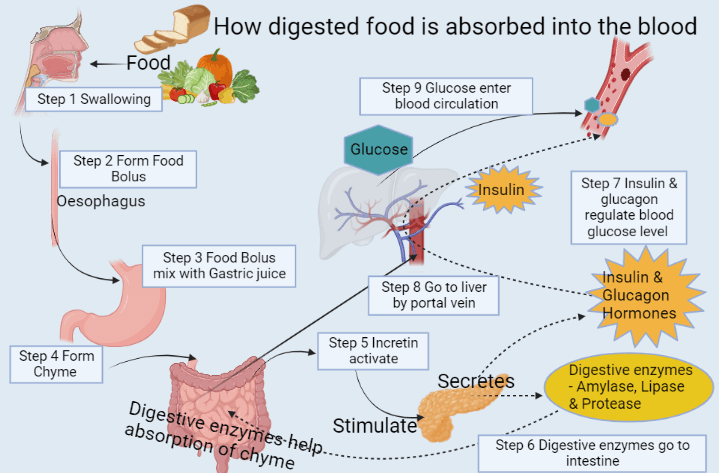
When you have a meal, it starts digestion from your mouth by salivary enzymes (like salivary amylase and lipase) and forms a Bolus.
This food bolus travels in your oesophagus pipe and reaches your stomach.
In the stomach, this food bolus completely breaks down by gastric juice like Hydrochloric Acid (HCL) that is secret from parietal cells. Here, the stomach starts churning and mixing food that converts into tiny pieces. This acidic food forms Chyme.
After that, it travels into your small intestine. As soon as food enters your small intestine, Incretins activate and secrets in your bloodstream.
These Incretins are gut hormones that are present in the epithelium layer of the intestine. There are some examples of Incretins and their functions –
- GLP-1(Glucagon-like Peptide-1) that decreases Glucagon and increases insulin hormone
- GIP (Gastric Inhibitory peptide or Glucose-dependent Insulinotropic) inhibits gastric emptying and increases satiety.
- Other Incretins like secretin, CCK (Cholecystokinin), and gastrin are digestive hormones.
After reaching blood circulation, these Incretins go to your Pancreas and stimulate it.
Incretins work as a messenger that signals to Pancreas to secret digestive enzymes (such as pancreatic amylase, protease and lipase) by Acinar cells and endocrine hormones (such as Insulin and Glucagon) by the Islet of Langerhans.
Digestive enzymes go to your small intestine through the pancreatic and bile duct. These pancreatic juices further break down food chyme and make it suitable for absorption.
After that, your food’s essential macro-nutrients (glucose, amino acids, monoglycerides, fatty acids etc.) get absorbed in the intestinal mucosa through SGLT 1 cotransporter.
SGLT 1 cotransporter is a sodium-glucose cotransporter that absorbs glucose and sodium in your intestinal mucosa.
Afterwards, it enters portal circulation and goes to your Liver by the portal hepatic vein.
In the Liver, these macronutrients get metabolised and converted into glucose, amino acids and cholesterol. Eventually, they circulate in your bloodstream.
On the other hand, endocrine hormones enter your bloodstream through the hepatic vein.
Before going to the bloodstream, these hormones go to your Liver by the hepatic portal vein, but they do not degrade in the Liver.
After passing through the Liver, Insulin and Glucagon reach systemic circulation that regulates your blood glucose level.
How do hormones regulate blood glucose levels?
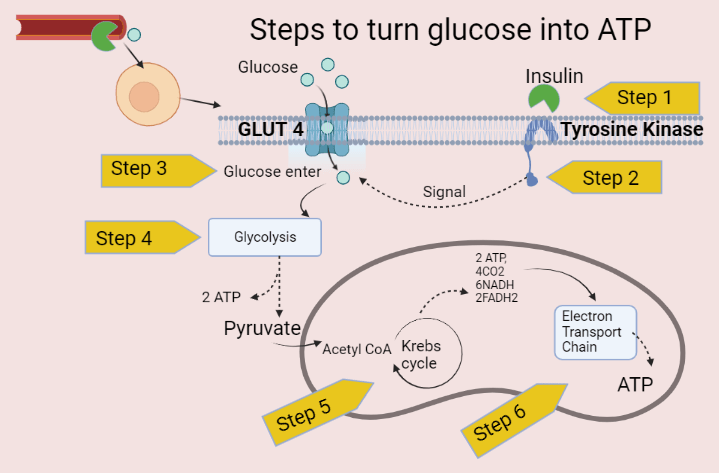
When glucose enters your systemic circulation, it goes to tissues, but glucose cannot enter your cells without Insulin.
Insulin helps in glucose uptake into cells. This means that Insulin increases the entry of glucose into your cells.
You would be thinking about how Insulin is released in our blood.
When you have a meal, incretins (GIP, GLP, etc.) release from your gut and go to your Pancreas. It stimulates Pancreas and releases Insulin.
Eventually, Incretins help to release Insulin. Due to this, Incretins are considered a natural anti-diabetic hormone.
After releasing Insulin from Pancreas, it goes to your blood circulation. It acts on the Tyrosine Kinase receptor that is present on the cell surface.
As soon as Insulin binds to the Tyrosine Kinase receptor, it facilitates the entry of glucose into cells.
Glucose also binds on the cell surface but acts on GLUT receptors or transporter like GLUT 1, GLUT 2, GLUT 3 and GLUT 4.
This is a normal process that occurs in the human body.
But our blood glucose level does not remain the same for an entire day; it fluctuates. Sometimes it gets high or low blood glucose levels.
To maintain this fluctuation, our Pancreas releases two crucial hormones – Insulin and Glucagon.
Let’s understand the significance of Insulin and Glucagon in blood glucose.
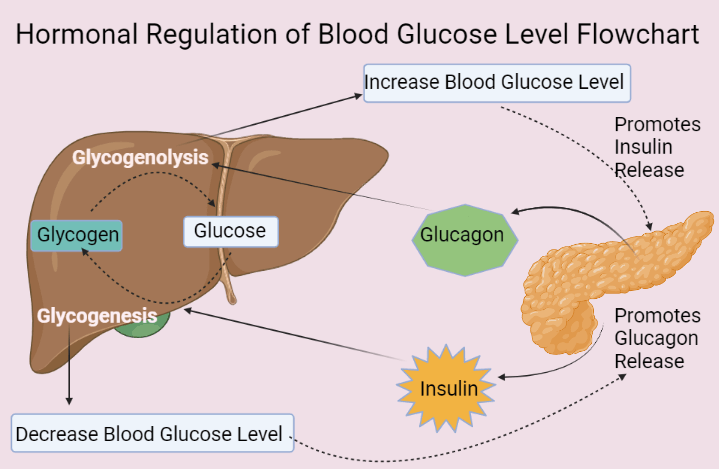
Role of Insulin
Suppose you have a high glucose content in your blood. This increased blood glucose level causes hyperglycaemia or diabetes mellitus.
In this condition, your Pancreas stops secreting Glucagon from alpha cells and starts secreting Insulin hormone from beta cells.
This insulin hormone goes to your Liver and promotes the Glycogenesis process.
This means that it converts the glucose into glycogen form.
Insulin also goes to your blood circulation and increases the glucose uptake in your cells.
Overall, it reduces the amount of glucose in the bloodstream during high blood glucose level conditions.
Role of Glucagon
Suppose you have a low glucose content in your blood. This decreased blood glucose level causes hypoglycaemia, which can be fatal.
In this condition, your Pancreas stops secreting Insulin from beta cells and starts secreting glucagon hormone from alpha cells. This glucagon hormone goes to your Liver and stimulates the Glycogenolysis process.
Usually, the Liver stores excess glucose in the form of glycogen by the Glycogenesis process.
It releases in emergencies (like starvation or hypoglycaemia) when you don’t have enough glucose in your blood.
Here, Glucagon helps break down the glycogen and release glucose through Glycogenolysis.
This Glycogenolysis releases glucose in your blood circulation and prevents low blood glucose or hypoglycaemia.
Role of Somatostatin
Sometimes Insulin and Glucagon get uncontrolled.
Overproduction of Insulin causes hypoglycaemia that decreases blood glucose levels. For example – Insulinoma (tumour of the Pancreas, nearby beta cells) and Insulin Resistance.
While the overproduction of Glucagon causes hyperglycaemia that increases blood glucose levels. For example – Glucagonoma (tumour of the Pancreas, nearby alpha cells).
There is a crucial role of somatostatin. This hormone controls the overproduction of insulin and glucagon hormones.
It inhibits the secretion of Insulin and Glucagon.
Somatostatin is also called the Universal inhibitor of a peptide hormone in pancreatic islets.
How is glucose oxidised to provide energy?
Our body needs energy. Whatever we eat eventually converts into energy.
When glucose circulates in your blood circulation, it has to go into your cells to provide energy.
Glucose enters your cell by GLUT receptors.
In the cell, glucose gets breakdown by the Glycolysis pathway in your cell’s cytoplasm.
In the Glycolysis pathway, your glucose molecules split into pyruvate molecules and release some energy as ATP.
The pyruvate is an end product of your Glycolysis pathway.
After converting into pyruvate from glucose, this pyruvate goes to the mitochondria part of a cell. Here, it enters the Citric acid cycle (or Krebs cycle).
In the Citric Acid Cycle, pyruvate gets converted into Acetyl CoA. This process produces carbon dioxide (CO2) and some energy as 2 ATP, 6 NADH and 2 FADH2.
This NADH and FADH2 enter ETC (Electron Transport Chain), which also occurs in mitochondria.
The primary role of ETC is to generate more energy in the form of ATP.
Do brain cells require Insulin for glucose uptake?
Insulin is a polypeptide hormone, and all polypeptide hormones are water-soluble.
Therefore, Insulin is a water-soluble hormone and does not cross lipid membranes.
Due to the hydrophilic property of Insulin, it cannot cross the blood-brain barrier, that is lipid membrane. So, Insulin does not enter your brain.
Although, the brain does not need Insulin because the brain contains GLUT 1 and GLUT 3 receptors. These types of GLUT receptors do not require Insulin for Glucose uptake in cells.
- GLUT 1 and GLUT 3 – Brain
- GLUT 2 – Pancreas, Liver and kidney
- GLUT 4 – Heart, Skeletal muscle, and Adipose tissue
What is the difference between insulin and glucagon hormone?
Glucagon is a counter-regulatory hormone for Insulin. If you have too much Insulin in your blood, there could be a chance of low blood sugar levels. In that case, Glucagon is released from Pancreas and goes to the Liver.
In the Liver, it stimulates the Glycogenolysis process, converting glycogen into glucose. After releasing glucose from the Liver, it enters your bloodstream and maintains glucose homeostasis.
|
Difference between Insulin and Glucagon |
||
| Characteristics | Insulin | Glucagon |
| Production | Alpha cells of pancreas | Beta cells of pancreas |
| Function | Lower the blood glucose level | Increase the blood glucose level |
| Hepatic Gluconeogenesis (formation of glucose) | Decrease | Increase |
| Hepatic glycogenesis (glycogen synthesis) | Increase | Decrease |
| Hepatic glycogenolysis (glucose synthesis) | Inhibit | Increase |
| Glucose uptake in muscle tissues | Increase glucose uptake | No response |
| Deficiency | Hyperglycaemia | Hypoglycaemia |
| Overproduction | Hyperinsulinemia due to insulin resistance or insulinoma | Hyperglucagonemia or glucagonoma |
Conclusion
We have seen how hormonal regulation of blood glucose levels occurs in the human body.
In this post, we discussed the role of insulin and glucagon hormones that regulate your blood glucose level.
Insulin and glucagon hormones play a critical role in maintaining blood glucose levels because these two hormones counterbalance each other to stabilize blood glucose.
When blood glucose falls, your Pancreas secretes glucagon hormone to raise blood glucose. Similarly, when blood glucose rises, your Pancreas secretes insulin hormone to decrease blood glucose.
It was all about the hormonal regulation of blood glucose levels.
Please share it if you found this post informative.
Have questions?
Ask in below comment box.
FAQ
Q 1. Which gland secretes Insulin and Glucagon?
The Pancreas is an organ that also acts as a gland that secretes insulin and glucagon hormones.
Q 2. Which hormone regulate blood sugar level?
Insulin and Glucagon are two crucial hormones that regulate blood sugar levels.
Q 3. What are the hormones secreted by the Pancreas?
Pancreas secretes some important endogenous hormones like Insulin, Glucagon, and Somatostatin. These hormones release in your blood circulation and regulate your glucose homeostasis.
Q 4. What is the main role of Insulin?
The primary purpose of Insulin is to increase glucose uptake into your cells and maintain the glucose content in your blood.


