What is the Difference Between Conjugated and Unconjugated Bilirubin?
 Posted On
Posted On
Contents
- Introduction
- What is bilirubin in a blood test?
- How is bilirubin formed from the breakdown of haemoglobin?
- What is unconjugated bilirubin? What does a high level of unconjugated bilirubin indicate?
- 1. Haemolytic Jaundice
- 2. Neonatal Jaundice
- 3. Genetic factors
- 4. Drug-induced unconjugated hyperbilirubinemia
- What is conjugated bilirubin? What causes high-level conjugated bilirubin?
- 1. Intrahepatic biliary duct obstruction
- 2. Extrahepatic Biliary Duct Obstruction
- What triggers cholestasis of pregnancy?
- What is the difference between Conjugated and Unconjugated Bilirubin?
- How to calculate conjugated and unconjugated bilirubin?
- Conclusion
- FAQ
- Q 1. What is the role of bilirubin?
- Q 2. What form of bilirubin is found in blood?
- Q 3. What is the difference between direct and conjugated bilirubin?
- Q 4. What is the difference between Conjugated and Unconjugated Hyperbilirubinemia?
- Q 5. What are the 3 types of jaundice?
- Q 6. Is jaundice from conjugated or unconjugated bilirubin?
Introduction
Are you curious to know the difference between conjugated and unconjugated bilirubin?
Whenever you have a liver problem, your doctor suggests a liver function test. You must have found conjugated and unconjugated bilirubin levels in your report.
Unconjugated bilirubin is a toxic product that forms after the expiry of red blood cells in the spleen. Whereas conjugated bilirubin is a non-toxic product that produces during metabolism in the liver.
This bilirubin test is essential in clinical practice to diagnose liver disease (such as Jaundice) and other health problems.
In this article, we will discuss bilirubin, metabolism of bilirubin, normal range of bilirubin, and its clinical relevance. Further, we will also know the difference between conjugated and unconjugated bilirubin.
Let’s get started.
What is bilirubin in a blood test?
Bilirubin is a biochemical parameter of your liver function test. Your doctor uses this tool to diagnose liver disease.
In the human body, bilirubin is a waste product of your hemoglobin produced during the red blood cells breakdown in the spleen.
Although bilirubin does not have a specific function, it is generally a component of bile juice. It is also called a bile pigment, which is yellow in color.
There are two forms of bilirubin in our blood.
One is unconjugated bilirubin, which forms during the breakdown of red blood cells, and the other is conjugated, which starts during metabolism in the liver.
How is bilirubin formed from the breakdown of haemoglobin?
Your red blood cell’s (RBCs) average life span is 120 days. After 120 days, RBCs have to be destroyed.
These cells go to your spleen. Here, the spleen acts as a lymphatic organ that plays a vital role in destroying old RBCs by phagocytosis. That’s why the spleen is also known as the “Graveyard of RBC“.
Generally, Red blood cells contain haemoglobin. It gets breakdown into “heme” and “globin”.
This “heme” converts it into biliverdin and then eventually converts it into bilirubin with the help biliverdin reductase enzyme.

This bilirubin is very toxic and lipid-soluble (or water-insoluble). This type of bilirubin is called unconjugated bilirubin.
Your body does not want to stay unconjugated bilirubin in your blood for long.
So, it gets metabolised in your liver and forms a water-soluble compound – conjugated bilirubin so that it can excrete quickly from your body.
Therefore, once unconjugated bilirubin enters your blood, it gets attached to albumin, which flows in your blood.
Here, albumin acts as a transporter that helps your unconjugated bilirubin move towards the liver.
As soon as unconjugated bilirubin enters your liver, it starts metabolizing it. Eventually, it converts the unconjugated bilirubin into conjugated bilirubin by conjugation process (especially glucuronidation reaction with UGT).
This conjugated bilirubin is less toxic, more polar and water-soluble. Conjugated bilirubin is also an excretory substance that comes out with your bile and travels through the bile duct.
Finally, it reaches the small intestine (duodenum). Then it goes to the large intestine, oxidised by some bacteria that convert into urobilinogen.
Urobilinogen is a final bilirubin product that excretes from the body through urine and faces.

What is unconjugated bilirubin? What does a high level of unconjugated bilirubin indicate?
The unconjugated bilirubin is a catabolic product of red blood cells. This non-conjugated compound is also known as indirect bilirubin.
So, indirect bilirubin means unconjugated bilirubin.
Your blood test report shows an indirect bilirubin normal range of 0.2 to 0.8 mg/dL, which may vary from lab to lab.
If you get your LFT done, you see a high unconjugated bilirubin (UCB) level above the reference range. This is called Unconjugated Hyperbilirubinemia.
You may have high UCB by these three possible mechanisms –
- Overproduction of bilirubin
- Decrease hepatic uptake of UCB
- Decrease conjugation in the liver
Some possible reasons or diseases associated with unconjugated hyperbilirubinemia –
1. Haemolytic Jaundice
Hemolytic anemia is the most common cause of the increased production of bilirubin.
In this type of anemia, you may have excess destruction of RBCs that cause high unconjugated bilirubin in the blood. The liver is unable to conjugate this high UCB quickly.
Due to this, UCB gets increased in your blood and deposited in your skin and sclera, reflecting yellowish in colour. You can see this classical clinical sign if serum bilirubin levels exceed 3 mg/dl.
This type of hemolytic Jaundice is also called Pre-Hepatic Jaundice because there is no direct involvement of the liver to cause Jaundice.
If you have Jaundice due to hemolysis, you should also go with some other laboratory tests like Hb (haemoglobin), LDH (Lactate dehydrogenase), and haptoglobin (haptoglobin is a protein that binds on free haemoglobin).
You would see some imbalance of biochemical parameters in your report –
- Decrease Hb
- Increase LDH
- Increase haptoglobin
2. Neonatal Jaundice
You must have seen Jaundice in a new-born baby.
When a child is born, its liver is tiny, and it takes time to mature the liver cells.
Because of the unmatured liver, it does not occur conjugation process. This causes high unconjugated bilirubin in new-born that leads to Jaundice. This is known as Neonatal Jaundice.
Although neonatal Jaundice is not life-threatening. If not treated well, it can be fatal.
Since UCB is toxic and lipid soluble. So, a lipid-soluble compound can cross the blood-brain barrier, which leads to brain damage.
This is called Bilirubin Induced Encephalopathy (or kernicterus).
Sometimes when you breastfeed your child, it may also increase the level of bilirubin; this is called Maternal Milk Jaundice.
Moreover, it may also cause Jaundice if you don’t breastfeed your baby because lactation failure may also cause Jaundice.
3. Genetic factors
Some genetic factors are also responsible for increasing the level of unconjugated bilirubin.
Suppose someone has a mutation in a gene of liver cells. In that case, that person may have high unconjugated bilirubin in the blood. It is most specific with variation in UDP-glucuronosyltransferase 1A1 (UGT1A1) gene that causes –
- Gilbert syndrome, and
- Crigler-Najjar syndromes type I or II
These rare genetic disorders reduce the conjugation process of unconjugated bilirubin and lead to hyperbilirubinemia.
4. Drug-induced unconjugated hyperbilirubinemia
You may have unconjugated hyperbilirubinemia if you are on certain medicines like –
- Aspirin (NSAIDs) and sulphonamides (antibiotic)
The free unconjugated bilirubin is generally attached to albumin in your blood.
Suppose you take a high dose of aspirin or sulphonamide medicines; these medicines compete with albumin.
So, Aspirin and sulphonamide get detached from the unconjugated bilirubin from albumin and attached to the albumin itself. Due to this, this free unconjugated bilirubin (or unbound bilirubin) gets increased in your blood.
This high unconjugated bilirubin may damage your brain (or kernicterus). It can be seen mostly in children that causes Reye Syndrome, mainly due to Aspirin.
- Novobiocin (antibiotic)
Novobiocin is an antibiotic that has the potential to cause unconjugated hyperbilirubinemia by interfering in bilirubin conjugation.
This medicine inhibits the conjugation enzyme UDP-glucuronosyltransferase (UGT).
- Protease inhibitors (antiretroviral drugs)
Protease inhibitors are antiretroviral drugs that are used in the treatment of HIV infection. But these medicines are highly associated with increased unconjugated bilirubin in your blood.
They also inhibit the conjugation enzyme UDP-glucuronosyltransferase (UGT), which leads to Jaundice.
Some examples of protease inhibitors include indinavir, saquinavir, ritonavir, etc.

What is conjugated bilirubin? What causes high-level conjugated bilirubin?
Conjugated bilirubin is generally formed after the glucuronidation of the unconjugated bilirubin.
The conjugation process occurs in your liver and converts your unconjugated bilirubin into conjugated bilirubin. This type of glucuronidation compound is also known as direct bilirubin.
In simple words, direct bilirubin means conjugated bilirubin.
Your blood test report shows the direct bilirubin normal range of 0.0 to 0.3 mg/dL, which may vary from lab to lab.
Suppose you find the direct bilirubin above the reference range, such as higher than 2 mg/dL or more than 20% of total bilirubin. In that case, elevated conjugated bilirubin indicates Conjugated hyperbilirubinemia.
This condition is most commonly seen in cholestatic liver disease.
Cholestatic is a medical condition where the flow of bile juice gets reduced or stopped. You may have this cholestatic liver disease in two forms – Intrahepatic and extrahepatic obstruction.
Let’s discuss this in detail –
1. Intrahepatic biliary duct obstruction
When bile juice gets prepared, it travels in narrow biliary tubes inside your liver. The network of these tiny thin tubes is known as Intrahepatic Biliary Duct.
If you get impairment or any obstruction in these tiny tubes, it will increase both conjugated and unconjugated bilirubin. In this condition, it cannot excrete bilirubin from the bile duct. This condition is called Intrahepatic Biliary Duct Obstruction (IHBDO).
Sometimes, it is also called Intrahepatic Jaundice.
The leading cause of intrahepatic duct obstruction is hepatocellular (or liver) injury. This liver injury may be due to –
- Autoimmune diseases such as primary biliary cholangitis (inflammation of the intrahepatic bile duct)
- Viral hepatitis
- Alcoholic hepatitis
It could be due to sepsis and exposure to bacterial infection. These things activate your immune system, releasing cytokines and interleukins (such as IL-1, IL-6, and alpha TNF).
These inflammatory chemicals go to your bile duct and make it shrink, restricting the flow of bile. As a result, conjugated bilirubin will not drain to the bile duct, and it goes back to your bloodstream. Moreover, it also hampers the conjugation process in your liver.
Eventually, it will increase the conjugated and unconjugated bilirubin levels in your blood.
Apart from elevated bilirubin, you will also notice a high level of ALP (Alkaline phosphatase) and GGT (gamma-glutamyl transferase).
Bile juice is a mixture of various components. Among these components, there are bile salts like Cholate and chenodeoxycholate.
In Intrahepatic Jaundice, the level of bile juice increases, leading to elevated bilirubin and bile salts in your blood. Due to this, you may have experienced the following sign and symptoms –
- Pruritus or itching due to high levels of bile salts
- Yellowish eye sclera and skin due to an elevated level of bilirubin
- Loss of appetite due to impaired metabolism
- Lemon yellow to apple green skin due to biliverdin if longstanding intrahepatic Jaundice
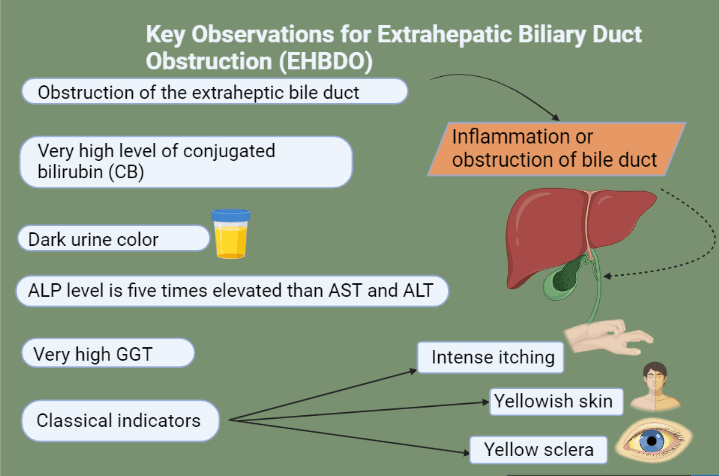
2. Extrahepatic Biliary Duct Obstruction
When bile juice leaves the liver, it travels in the wide bile duct to reach the small intestine. These bile ducts that present outside the liver are called Extrahepatic Biliary Duct.
Suppose you get any fibrosis or obstruction in these external bile ducts, leading to inflammation and swelling.
This inflammation causes blockage and reduces the flow of bile juice. In this condition, your bile juice cannot travel in the bile duct. As a result, it increases the level of conjugated bilirubin.
You will not have a problem in your conjugation process because your liver cells work well. Due to obstruction of the bile duct, you will have conjugated hyperbilirubinemia.
This type of blockage in the external bile duct of the liver is called Extrahepatic Biliary Duct Obstruction (EHBDO).
It is also known as Extrahepatic Jaundice. The leading cause of extrahepatic Jaundice is
- Choledocholithiasis (stone in the bile duct)
- Benign bile duct strictures
- Cholangiocarcinoma (cancer in the bile duct)
The laboratory LFT report shows a high level of direct bilirubin, ALP and GGT.
Also read, SGOT and SGPT In Liver Function Test
What triggers cholestasis of pregnancy?
You must have seen an itching problem in pregnant women that usually occurs in late pregnancy. This itching problem in pregnancy indicates a liver problem, and it is called Intrahepatic Cholestasis of Pregnancy (ICP).
In the last pregnancy stage, pregnancy hormones (such as estrogen and progesterone) are at their peak.
The high surge of estrogen stops bile flow into the bile duct. As a result, you will have conjugated and unconjugated hyperbilirubinemia.
This elevated bilirubin gets deposited in your skin, and you may have pruritus (or itching problem).
Some key markers can also be seen in ICP conditions, like elevated ALP and GGT.
What is the difference between Conjugated and Unconjugated Bilirubin?
Here, I have compared these two forms of bilirubin in the table below. You can see the significant difference between conjugated and unconjugated bilirubin.
| Features | Unconjugated bilirubin | Conjugated bilirubin |
| Description | Does not have conjugation | Conjugation occurs |
| Another name | Indirect bilirubin | Direct bilirubin |
| Solubility | Lipid soluble | Water soluble |
| Type of compound | Non-polar | More polar |
| Toxicity | Toxic | Non-toxic |
| Protein carrier | Bind with albumin for transportation | Does not bind with any protein |
| Normal range in adult | 0.2 to 0.8 mg/dL | 0.0 to 0.3 mg/dL |
| High concentration in blood | Unconjugated hyperbilirubinemia | Conjugated hyperbilirubinemia |
| Clinical relevance | Normal urine colour during unconjugated hyperbilirubinemia | Dark urine indicates conjugated hyperbilirubinemia |
| Classical indicators | Scleral icterus and yellowish skin | Pruritus, scleral icterus and yellowish skin |
| Other lab parameters | AST, ALT and ALP levels are normal in unconjugated hyperbilirubinemia | Very high ALP and GGT level in conjugated hyperbilirubinemia |
How to calculate conjugated and unconjugated bilirubin?
If you sum the conjugated and unconjugated bilirubin, it would be your total bilirubin.
It means the total bilirubin is a combination of conjugated and unconjugated bilirubin.
Total bilirubin = conjugated (or direct) bilirubin + unconjugated (or indirect) bilirubin
= 0.0 to 0.3 mg/dL + 0.2 to 0.8 mg/dL
= 0.2 to 1.1 mg/dL
The normal range of total bilirubin is 0.2 – 1.1 mg/dl for adults. You can calculate your other bilirubin parameters by this formula. For example,
- If you get high indirect bilirubin after subtracting total bilirubin from direct bilirubin, it indicates Prehepatic jaundice.
Indirect bilirubin = (total bilirubin minus direct bilirubin level)
= 2.5 – 0.3 = 2.2 mg/dl
- If you get an elevated direct bilirubin level after subtracting total bilirubin from indirect bilirubin, it indicates Post-hepatic Jaundice.
Direct bilirubin = (total bilirubin minus indirect bilirubin level)
= 4 – 1 = 3 mg/dl
- If you find elevated both indirect and direct bilirubin that represents higher total bilirubin. It indicates Intrahepatic jaundice.
Total bilirubin = direct bilirubin + indirect bilirubin
= 1.1 + 2.1 mg/ dl
=3.2 mg/dl
Conclusion
Bilirubin is a natural by-product of red blood cells with yellowish pigment. It is considered a waste product, and its elimination is essential.
We have seen two types of bilirubin – conjugated and unconjugated.
Clinically, you will have a medical condition if a bilirubin level is elevated. For example –
- Excess unconjugated bilirubin indicates Pre-Hepatic Jaundice
- Excess conjugated bilirubin indicates EHBDO or Post Hepatic Jaundice
- Excess of both conjugated and unconjugated bilirubin indicates IHBDO or Intrahepatic Jaundice
If you find any imbalance of bilirubin in your LFT report, you must consult your doctor. Your doctor will clinically correlate the imbalanced bilirubin with your symptoms.
It was an informative post about conjugated and unconjugated bilirubin.
Have questions?
Let me know in the comments below. I will try my best to answer all of them.
FAQ
Q 1. What is the role of bilirubin?
When your red blood cells get expire, it produces bilirubin. Simply, bilirubin is a waste product of your haemoglobin. Although, bilirubin does not have a specific role in your body. Some studies suggest that it acts as an antioxidant in the human body.
Q 2. What form of bilirubin is found in blood?
There are two forms of bilirubin in our blood –
- Unconjugated (indirect) bilirubin – bound with albumin protein
- Conjugated (direct) bilirubin – formed in the liver after metabolism
Q 3. What is the difference between direct and conjugated bilirubin?
Direct bilirubin is also known as conjugated bilirubin. This type of bilirubin forms after conjugation with glucuronic acid in your liver.
Q 4. What is the difference between Conjugated and Unconjugated Hyperbilirubinemia?
An excess amount of conjugated bilirubin in your blood is called conjugated hyperbilirubinemia. This indicates post-hepatic jaundice. While the elevated unconjugated bilirubin in your blood is called unconjugated hyperbilirubinemia. This means prehepatic jaundice.
Q 5. What are the 3 types of jaundice?
You may have jaundice in three forms –
- Pre-hepatic jaundice (due to haemolysis)
- Intrahepatic jaundice (due to hepatocellular injury)
- Post hepatic Jaundice (due to inflammation or obstruction in the bile duct)
Q 6. Is jaundice from conjugated or unconjugated bilirubin?
You may have an imbalance of bilirubin in different types of jaundice, like –
- Pre-hepatic jaundice – elevation of unconjugated bilirubin
- Intrahepatic jaundice – elevation of conjugated and unconjugated bilirubin
- Post hepatic jaundice – elevation of conjugated bilirubin



