Antidiabetic Drug Classification and Mechanism of Action: algorithm for management of diabetes mellitus
 Posted On
Posted On
Contents
- Introduction
- What are antidiabetic drugs?
- What are the classifications of antidiabetic drugs with examples?
- Injectable Diabetes Medications
- Oral Hypoglycemic Drugs (or Antidiabetic Agents)
- Which drugs are Biguanides?
- Mechanism of action of metformin
- Side effects of metformin
- Dosage of metformin
- What drugs are Sulphonylureas? What can be the role of Sulphonylureas in treatment of diabetes?
- Sulfonylureas mechanism of action
- Side effect of Sulphonylureas
- Dosage of Sulphonylureas
- What are examples of meglitinide analogues? Why meglitinides are better than sulfonylureas?
- Meglitinide’s mechanism of action
- Benefits of Meglitinides
- Dosage of Meglitinides
- What is the mechanism of thiazolidinediones? Is pioglitazone safe to take for diabetes?
- Pioglitazone mechanism of action
- Pioglitazone side effects and contraindications
- Pioglitazone benefits
- Which drugs are DPP-4 inhibitors? How do DPP-4 inhibitors work?
- DPP-4 inhibitor’s mechanism of action
- DPP-4 inhibitors brand names
- What are currently used alpha-glucosidase inhibitors? What is the clinical role of these drugs in diabetes mellitus?
- Alpha-glucosidase inhibitor’s mechanism of action
- Alpha-glucosidase inhibitor’s side effects
- Acarbose and voglibose dosage
- What are the most common SGLT2 inhibitors? How do SGLT2 inhibitors work?
- SGLT2 inhibitor’s mechanism of action
- SGLT2 inhibitor’s side effects
- What are insulin analogues? What are the different types of insulin names?
- 1. Short-acting insulin
- 2. Ultra short-acting insulin
- 3. Intermediate-acting Insulin
- 4. Long-acting insulin
- 5. Ultra-long acting insulin
- 6. Premixed Insulin
- Combination of intermediate and ultra-short-acting insulin
- Combination of intermediate and short-acting insulin
- Combination of ultra-short and ultra-long-acting insulin
- What is the role of liraglutide and exenatide in diabetes mellitus?
- What is the pharmacological management of diabetes mellitus?
- STEP 1 – Mono-therapy
- STEP 2 – Dual therapy
- STEP 3 – Triple Therapy
- STEP 4 – Injectable with combinations
- Conclusion
- FAQ
- Q 1. What is the first drug of choice for diabetes?
- Q 2. Which antidiabetic drug class lead to glycosuria?
- Q 3. What is the new drug for diabetes?
- Q 4. Is repaglinide safe for kidneys?
- Q 5. Is linagliptin safe for kidneys?
Introduction
You must have a diabetic person in your family or relatives. They would be taking different diabetes medications. Today, we will get to know the complete antidiabetic drug classification.
Lifestyle modifications (such as diet control and exercise) are the gold standard for treating diabetes.
We should add the best diabetic diet plan, such as low glycemic index foods, low glycemic load foods, high protein food, proper fluid intake, etc.
Suppose the lifestyle changes do not work and your blood sugar is still high. In that case, antidiabetic drugs should be added to your diabetes treatment.
It does not mean you should stop exercising and not eating healthy foods. You have to add on medicine with healthy lifestyle activities.
This article will explore various antidiabetic drug classifications, their mechanism of action, uses, side effects and dosage.
Moreover, we will understand what medicines are preferable and suitable for treating diabetes mellitus.
Let the article be started.
What are antidiabetic drugs?
Antidiabetic drugs are those drugs that reduce blood sugar levels by releasing insulin or overcoming insulin resistance. It makes your blood sugar level in normal ranges –
These drugs resolve diabetic symptoms by decreasing blood sugar levels, such as –
- Decrease tiredness
- Control excessive urination
- Control excessive eating
- Control intense thirst
- Prevent weight loss
- Stop dehydration
Antidiabetic drugs also prevent diabetic complications such as
- Macrovascular complications – Reduce the risk of Cerebrovascular Disease (CVD), Coronary artery disease (CAD), Peripheral vascular disease (PVD), and Renovascular Disease (RVD)
- Microvascular complications – Reduce the risk of Diabetic neuropathy, Diabetic nephropathy, and Diabetic retinopathy
What are the classifications of antidiabetic drugs with examples?
Antidiabetic drugs have been classified into two forms: injectable and oral antidiabetic drugs (OHA – Oral Hypoglycemic Agents)
Injectable Diabetes Medications
Injections are not the first choice drug for diabetes. They are last-line medication options if your diabetes is getting uncontrolled. You can be given the following injections –
- Insulin analogues
- Incretins based drugs such as GLP-1 analogs (Exenatide and Liraglutide)
Oral Hypoglycemic Drugs (or Antidiabetic Agents)
The major drawback of insulin analogues is that it is given by injection. That’s why oral hypoglycaemic medicines are preferable and commonly used in type-2 diabetes mellitus treatment.
Oral hypoglycemic agents are quite effective to control your high blood glucose levels. It only works on type 2 diabetes mellitus.
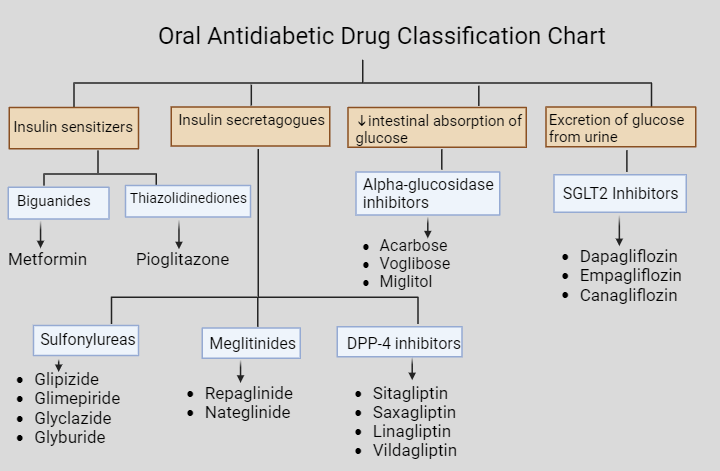
Currently, there are 4 ways/groups of oral antidiabetic medicines to reduce high blood sugar levels –
- Insulin sensitizers
- Insulin secretagogues
- Decrease intestinal absorption of glucose
- Excretion of glucose from urine
Oral antidiabetic medications have been classified into 7 classes, such as –
1. Biguanides
2. Thiazolidinediones
3. Sulfonylureas
4. Meglitinides
5. DPP-4 inhibitors
6. Alpha-glucosidase inhibitors
7. SGLT2 Inhibitors
|
Groups |
Classes |
Examples of medicines |
|
Insulin sensitizers |
Biguanides |
Metformin |
|
Thiazolidinediones |
Pioglitazone |
|
|
Insulin secretagogues |
Sulfonylureas |
Glipizide, Glimepiride, Glyclazide, Glyburide |
|
Meglitinides |
Repaglinide, Nateglinide |
|
|
DPP-4 inhibitors |
Sitagliptin, Saxagliptin, Linagliptin, Vildagliptin |
|
|
Decrease intestinal absorption of glucose |
Alpha-glucosidase inhibitors |
Acarbose, Voglibose Miglitol |
|
Excretion of glucose from urine |
SGLT2 Inhibitors |
Dapagliflozin, Empagliflozin, Canagliflozin |
Which drugs are Biguanides?
Metformin is a drug that belongs to the biguanide category.
Everyone knows this drug because metformin tablet is the most commonly prescribed medicine for type 2 diabetes mellitus (T2DM). This is the initial drug where diabetes treatment should be started.
It is considered a first-line drug in treating type 2 diabetes mellitus.
Let’s know the pharmacology of metformin drug –
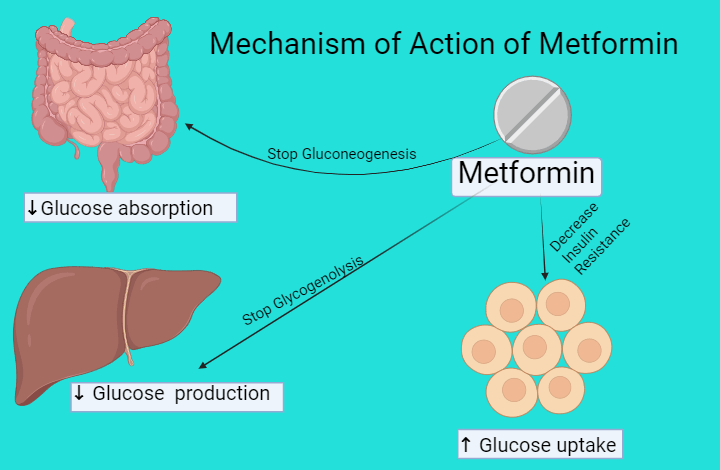
Mechanism of action of metformin
Metformin drug works in three ways –
- Decrease glucose absorption from the intestine
Metformin reduces gluconeogenesis. This means it decreases the absorption or formation of a new glucose molecule (e.g., protein) from the intestine.
- Decrease glucose production in the liver
Metformin reduces hepatic glycogenolysis. This means that it decreases the breakdown of glycogen, which converts into glucose and decreases glucose transport from the liver to the blood.
- Increase insulin sensitivity and glucose uptake in cells
Metformin helps to reduce insulin resistance. This drug activates Insulin, which helps to transport glucose molecules from blood to cells.
Side effects of metformin
The main side effects of metformin are related to the gastrointestinal tract, which is very common. This medicine can cause diarrhoea, bloating, flatulence, nausea, etc.
You might have dangerous side effects if you are using metformin. Lactic acidosis has been reported due to the use of excessive metformin doses.
This side effect could be fatal if your kidney and liver are compromised.
Metformin can also cause vitamin B12 deficiency. You may need to add vitamin B12 supplements along with metformin.
Dosage of metformin
The maximum dosage of metformin per day is 2000 mg. It would be best if you do not go beyond this dose.
Initially, your diabetes treatment should be started at 500 mg twice daily. It could be increased up to 1000 mg twice if diabetes is uncontrolled.
This drug can be combined with other antidiabetic classes like sulphonylureas, DPP-4 inhibitors, SGLT2 inhibitors, Meglitinides, thiazolidinediones, and alpha-glucosidase inhibitors.
You can take metformin just after having your meal.
What drugs are Sulphonylureas? What can be the role of Sulphonylureas in treatment of diabetes?
You must have heard the names of diabetic medicines which begin with “Gli”, like Glimepride, Gliclazide, Glibenclamide, and Glipizide.
These drugs are second-generation of sulphonylureas. The first generation of sulphonylureas, such as tolbutamide and chlorpropamide, are rarely used.
The sulphonylureas have a crucial role in the treatment of T2DM by releasing insulin from the pancreas.
These drugs are also known as Insulin Secretagogous.
Suppose you are intolerant of metformin. In that case, you can use sulphonylureas alone.
It can also be used in combination with metformin.
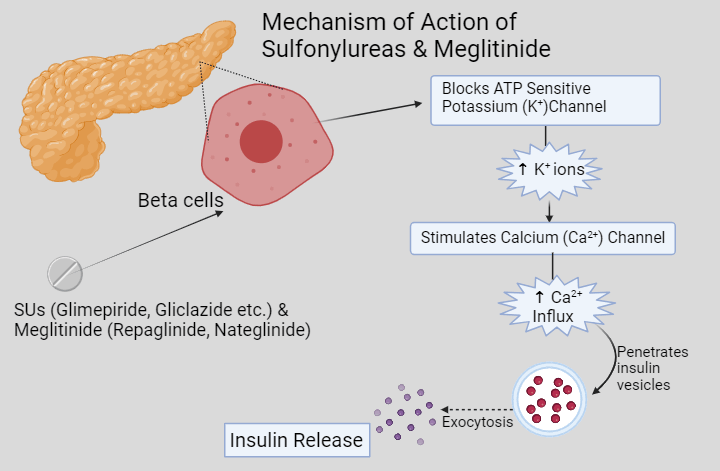
Sulfonylureas mechanism of action
When you take any sulphonylureas drug. They go to your pancreas and stimulate beta cells.
Here, it blocks the ATP-sensitive potassium (K+) channel. Due to this, a high concentration of potassium in your beta cells stimulates the calcium channel.
As soon as the calcium channel opens, it starts letting the influx of calcium ions. This increased influx of calcium ions penetrates the large, dense core vesicles where insulin is stored.
In this process of depolarisation, exocytosis takes place, and insulin is secreted. Overall, sulphonylureas help to secrete insulin. That’s why it is called Insulin Secretagogues.
After releasing insulin, it goes to the liver by the hepatic portal vein. Eventually, insulin reaches the central blood circulation.
Here, insulin goes to cells and binds to the Tyrosine Kinase receptor. After that, it lets the glucose come inside cells by GLUT-4 transporters.
Side effect of Sulphonylureas
You may have hypoglycaemia and weight gain-like side effects during sulphonylureas therapy.
Hypoglycemia was very common in first-generation sulphonylureas like tolbutamide and chlorpropamide.
The risk of hypoglycaemia is lower in newer sulphonylureas drugs like glimeride, gliclazide, etc.
Dosage of Sulphonylureas
It is usually recommended to start with a low dose, such as glibenclamide 2.5 mg, glimepiride 2 mg, gliclazide 30 mg, etc.
The dose of sulphonylureas can be increased every two weeks if your glycemic pattern is not controlled well.
It would be best if you take sulphonylureas 30 min before each meal once or twice a day as needed.
What are examples of meglitinide analogues? Why meglitinides are better than sulfonylureas?
Meglitinides are also effective oral hypoglycaemic drugs. There are two medicines in this category, such as repaglinide and nateglinide.
Repaglinide is considered a superior and preferable drug because of better glycemic control. It effectively controls elevated post-prandial blood sugar (PPBS) in T2DM.
These drugs have a good reduction in HbA1C, around 0.2 to 1.5%.
According to current guidelines, meglitinides are not recommended as part of an oral diabetes treatment regimen. Still, they may be used instead of sulfonylureas in selected patients.
Meglitinides can be used if someone has an allergy or is intolerant of sulphonylureas. It can also be used in kidney disease patients who have T2DM.
Meglitinide’s mechanism of action
Meglitidines have similar mechanisms to Sulphonylureas. They block the potassium channel and secrete insulin. These medicines are also known as Insulin Secretagogues.
Benefits of Meglitinides
- Repaglinide is the safest and most well-tolerated drug in chronic kidney disease.
- A safe and effective drug in an elderly diabetic patient
- Well-controlled post-prandial blood glucose (PPBG) level
- Quickly absorbed in the bloodstream
- Fast onset of action
- Lower risk of hypoglycaemia
Dosage of Meglitinides
This class of medicines should be taken 10 minutes before each meal to control your PPBS level.
The recommended dose range of repaglinide is 0.5 mg to 4 mg. It can be increased up to 16 mg as needed.
What is the mechanism of thiazolidinediones? Is pioglitazone safe to take for diabetes?
Thiazolidinediones (TZDs) are also known as “Glitazones”. Glitazones are the second or third-line treatment option for type 2 diabetes mellitus. It includes rosiglitazone and pioglitazone.
In 2010, Rosiglitazone was banned in many countries due to increasing life-threatening risks such as myocardial infarction, CHF, stroke and death.
These drugs have been completely withdrawn from European countries like Germany and France due to increased risk of bladder cancer and cardiovascular problems.
Currently, only pioglitazone is available in some countries like India. It is used as a mono-therapy in case of intolerance of metformin.
If diabetes is uncontrolled, then combinations can be used of pioglitazone with other antidiabetic drugs –
- Dual therapy (Pioglitazone + Metformin, or Sulphonylureas, or DPP-4 inhibitors)
- Triple therapy (Metformin + Pioglitazone + SGLT2 inhibitors) or (Metformin + Sulfonylurea + Pioglitazone)
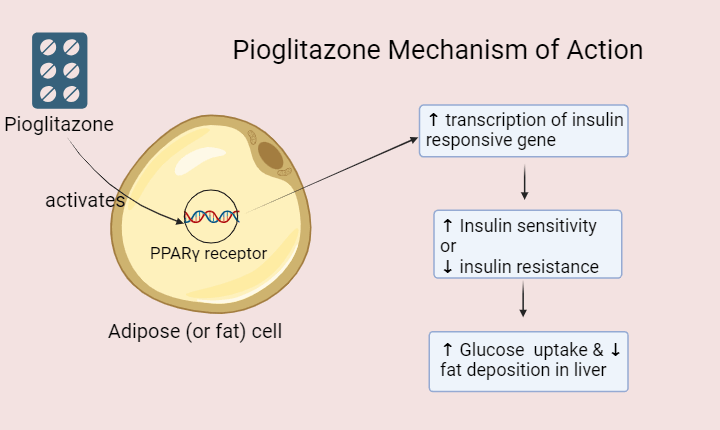
Pioglitazone mechanism of action
Pioglitazone drug works on the nuclear receptor, which stimulates PPAR- γ (peroxisome proliferator-activated receptor gamma).
PPAR- γ receptors are mainly present in fat cells. It alters the transcription of several genes and enhances GLUT4 expression, improving glucose entry into fat cells.
Overall, it reduces insulin resistance by increasing insulin sensitivity.
Pioglitazone side effects and contraindications
The most common side effects of pioglitazone are fluid retention and weight gain. You may notice swelling in your ankles if you are on pioglitazone.
You should avoid pioglitazone if you have a history of heart disease because it may worsen the condition of CHF (Congestive Heart Failure).
The liver dysfunctions have been reported by pioglitazone. So, you may require monitoring of LFT (Liver function test).
According to a study, pioglitazone is also associated with an increased risk of bone fractures, especially in older women.
Pioglitazone has lack of safety data in pregnancy. So, you should avoid this drug during pregnancy.
Pioglitazone benefits
Pioglitazone effectively controls elevated blood sugar levels if there is a clear case of insulin resistance. Let’s know it’s crucial benefits –
- Well-tolerated drug in T2DM
- Decrease TG (triglyceride) level
- Increase HDL level
- Less hypoglycaemic episodes
Which drugs are DPP-4 inhibitors? How do DPP-4 inhibitors work?
DPP-4 inhibitors are considered newer antidiabetic drugs. These drugs are also called “Gliptins” because these drugs end with the “gliptins” word. For examples –
- Sitagliptin
- Saxagliptin
- Linagliptin
- Vildagliptin
- Teneligliptin
If metformin is intolerant, your doctor can start DPP4 inhibitors as a mono-therapy (single drug therapy).
In case diabetes is uncontrolled, then combinations can be used of DPP-4 inhibitors with other antidiabetic drugs –
- Dual therapy (DPP4 inhibitors + metformin, or sulphonylureas, or pioglitazone)
- Triple therapy (Metformin + Sulfonylurea + DPP4 inhibitors)
DPP-4 inhibitor’s mechanism of action
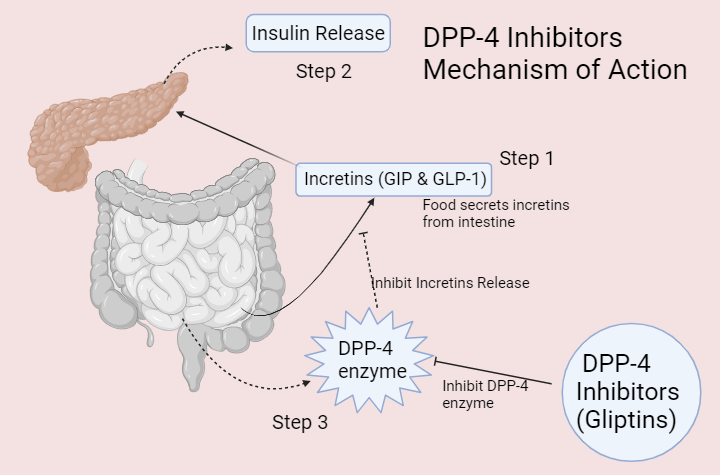
Taking food stimulates incretins like GIP (gastric inhibitory polypeptide) and GLP-1 (glucagon‐like peptide‐1).
These incretins go to the pancreas and get the insulin secreted.
But, you might have a problem when DPP-4 (Dipeptidyl-peptidase 4) enzymes are released. These DPP-4 enzymes inhibit the release of incretins and stop insulin secretion.
That’s why researchers have made a molecule that inhibits the DPP-4 enzyme. They launched DPP-4 inhibitors. These drugs are also insulin secretagogous.
DPP-4 inhibitors are those drugs that inhibit Dipeptidyl-peptidase 4 enzyme and release incretins like GIP and GLP-1. These incretins help to release insulin to control high blood glucose levels.
DPP-4 inhibitors brand names
There are some popular brand names for DPP-4 inhibitor drugs –
- Sitagliptin (Januvia)
- Saxagliptin (Onglyza)
- Linagliptin (Trajenta)
- Vildagliptin (Galvus)


Gliptins are commonly used in fixed-dose combinations with metformin drugs like –
- Janumet (Sitagliptin 50 mg and metformin hydrochloride 500 mg/1 gm)
- Kombiglyze XR (saxagliptin 5 mg and metformin HCl 500 mg/1 gm extended-release)
- Trajenta Duo (Linagliptin 2.5 mg and metformin hydrochloride 500 mg)
- Galvus Met (Vildagliptin and metformin HCL 500 mg/1 gm)
What are currently used alpha-glucosidase inhibitors? What is the clinical role of these drugs in diabetes mellitus?
Currently, Acarbose and Voglibose are the classical alpha-glucosidase inhibitors used to treat T2DM.
Suppose you are newly diagnosed with type 2 diabetes mellitus. And, your post-prandial blood glucose is not controlled with diet or exercise. In that case, this drug can also be used as a first-line drug.
It can also be used with metformin and other antidiabetic drugs.
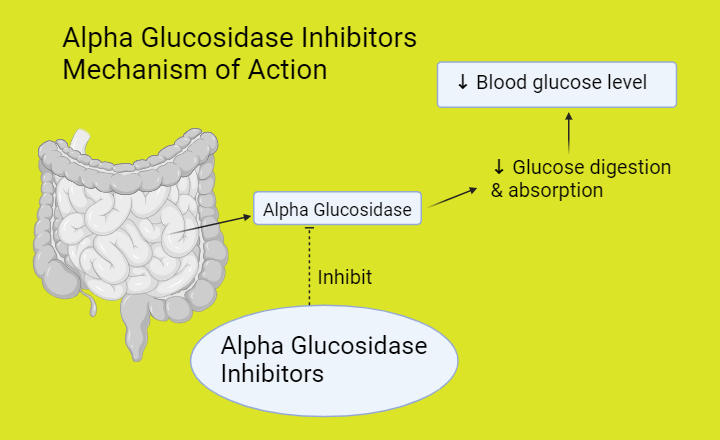
Alpha-glucosidase inhibitor’s mechanism of action
Typically, Alpha-glucosidase is an enzyme in our intestinal brush border.
This enzyme is released from the small intestine when we eat carbohydrates. It helps to break down carbohydrates in the simplest form, like glucose.
In diabetes conditions, this alpha-glucosidase enzyme increases the process of glucose digestion and absorption. This is not good in hyperglycaemic states.
Here, alpha-glucosidase inhibitors (such as acarbose and voglibose) inhibit the alpha-glucosidase enzyme. It delays the process of digestion and absorption of carbohydrates.
Eventually, these drugs decrease glucose absorption in the bloodstream and reduce blood glucose levels.
Alpha-glucosidase inhibitor’s side effects
The unabsorbed carbohydrates may cause abdominal bloating, cramping, increased flatulence, or diarrhoea.
You may have these side effects if you are on voglibose or acarbose.
Acarbose and voglibose dosage
You may take acarbose 50 to 100 mg or voglibose 0.2 to 0.3 mg thrice a day before the beginning of each meal.
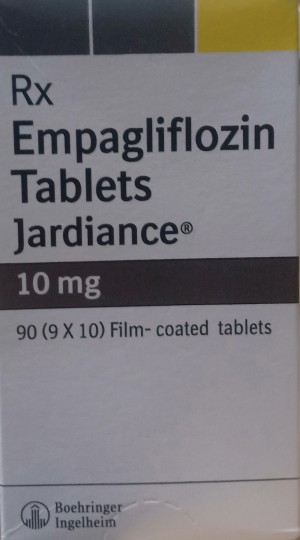
What are the most common SGLT2 inhibitors? How do SGLT2 inhibitors work?
SGLT2 inhibitors are newer antidiabetic drugs that help to treat type 2 diabetes mellitus.
They are also known as Gliflozins because these medicines end with “gliflozin”, word such as
- Dapagliflozin
- Empagliflozin
- Canagliflozin
This drug class can be used as a mono-therapy if metformin is intolerant or contraindicated.
In case of uncontrolled glycemic pattern, it should be started in combinations as a –
- Dual therapy (SGLT2 inhibitors + metformin, or sulphonylureas)
- Triple therapy (Metformin + Sulfonylurea + SGLT2 inhibitors) or (Metformin + Pioglitazone + SGLT2 inhibitors)
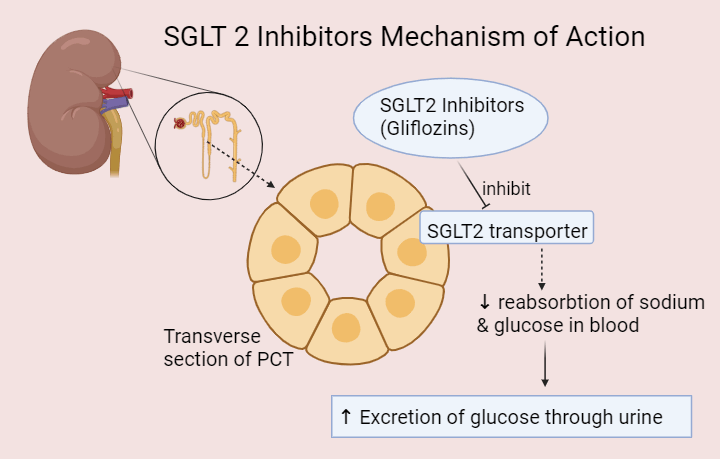
SGLT2 inhibitor’s mechanism of action
SGLT2 inhibitors have a novel and unique mechanism of action.
In a healthy person, there are SGLT-2 co-transporters or pumps in their kidney’s nephron. The full form of SGLT is Sodium Glucose Co-Transporter.
These transporters act as symporters that reabsorb sodium and glucose in your blood during urine formation.
In diabetes mellitus, re-absorption of glucose and sodium is not good, which may worsen your diabetic condition.
Here, SGLT2 inhibitors inhibit the SGLT2 co-transporters that excrete the sodium and glucose through urine.
Due to this unique mechanism, it significantly reduces blood glucose levels.
SGLT2 inhibitor’s side effects
You may have the following side effects during gliflozins therapy –
- Frequent urination
- Dehydration and hypotension
- Weight loss
- Hypoglycemia
- Excessive thirst and frequent urination
- Risk of foot amputations
- Risk of bone fractures


What are insulin analogues? What are the different types of insulin names?
Insulin shots are the last-line medication option to control high blood sugar levels.
Insulin injections are used to management of Type 1 (T1DM) and Type 2 Diabetes Mellitus (T2DM).
If you don’t have enough natural insulin, synthetic insulin should be given to you.
This synthetic insulin is called Insulin analogue.
Insulin analogue imitates the body’s standard insulin release patterns.
Insulin analogue injections are made using the pancreas of pigs (pork) and cows (beef). They can also be prepared by recombinant DNA technology.
In recombinant DNA technology, scientists use human pancreatic genes in E. coli (Escherichia coli) bacteria. They make insulin analogue.
There are different insulin types for diabetes. Some insulin analogues control the peak of glucose concentration; that insulin is called Bolus Insulin.
Bolus insulin is fast-acting insulin that immediately releases in your bloodstream and controls high blood sugar levels. They are given immediately just before your meal.
Conversely, those insulin analogues that maintain your blood sugar level for a long time are called Basal Insulin.
Basal Insulin is slow-acting or long-acting insulin. They release slowly in your bloodstream. When you take basal insulin, your blood glucose level remains steady throughout the day and night.
Let’s know the different types of insulin preparations –
1. Short-acting insulin
Regular Insulin or soluble Insulin is an example of short-acting insulin. This is a type of Bolus Insulin. This insulin preparation is in Human Actrapid Injection at 40 IU/ml.
If you see the cartridge or vial of short-acting insulin, it would be a clear appearance.
The onset of action is 30 mins, and the duration is 6 to 8 hours of regular insulin.
This means that regular insulin takes 30 mins to reach your blood circulation after subcutaneous injection and remains in your blood for 6 to 8 hours.
It shows the maximum effect (peak) in 2 to 3 hours.
You need to take Regular Insulin 30 minutes before a meal.
This is the limitation of Short-acting Insulin. It is not always possible to inject insulin before 30-minute meal. It reduces patient compliance and does not significantly reduce PPBG levels.
Other insulin preparations have been designed to overcome this problem, such as ultra-short, intermediate, long, and ultra-long-acting Insulin Injections.
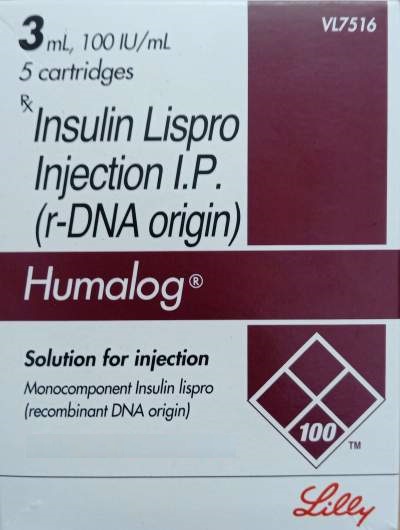
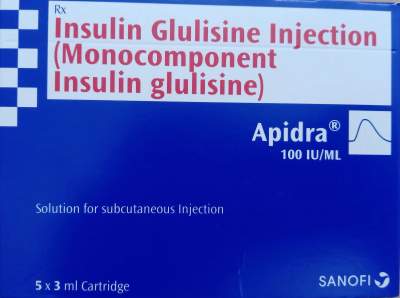
2. Ultra short-acting insulin
The most common type of insulin injection is ultra-short-acting insulin. This injection reduces the limitation of Regular Insulin (or Short-acting insulin).
It is a clear appearance.
It quickly absorbs in your bloodstream within 5 to 15 mins (onset of action). The duration of action is 2 to 4 hours.
You need to prepare your meal and take a shot of ultra-short-acting insulin. It is an effective bolus insulin because it significantly reduces elevated blood glucose level spikes or PPBG.
Examples of ultra-short-acting Insulin are Lispro, Aspart and Glulisine. You might have seen –
- Insulin Lispro in Humalog 100.
- Insulin Aspart in NovoRapid and NovoLog
- Insulin Glulisine in Apidra Solostar

3. Intermediate-acting Insulin
Intermediate-acting insulin is a Basal Insulin that keeps your blood sugar level stable when fasting, such as while you sleep.
An example of intermediate Insulin is Isophane. It is also known as NPH (Neutral Protamine Hagedorn) Insulin.
Isophane is mainly used to make premixed insulin. It is compatible to mix with short or rapid short-acting insulin.
You can easily identify this type of insulin. When you see the vial or cartridge of intermediate-acting insulin, it would have a cloudy appearance.
The onset of action is 60 to 90 min. It will reach a maximum concentration or peak in 8 to 10 hours. It will remain in your body for 20 to 24 hours.
You might need to inject Isophane insulin subcutaneously (s.c.) once or twice daily.
Isophane or NPH is available in the market with Huminsulin and Humulin N brand names.
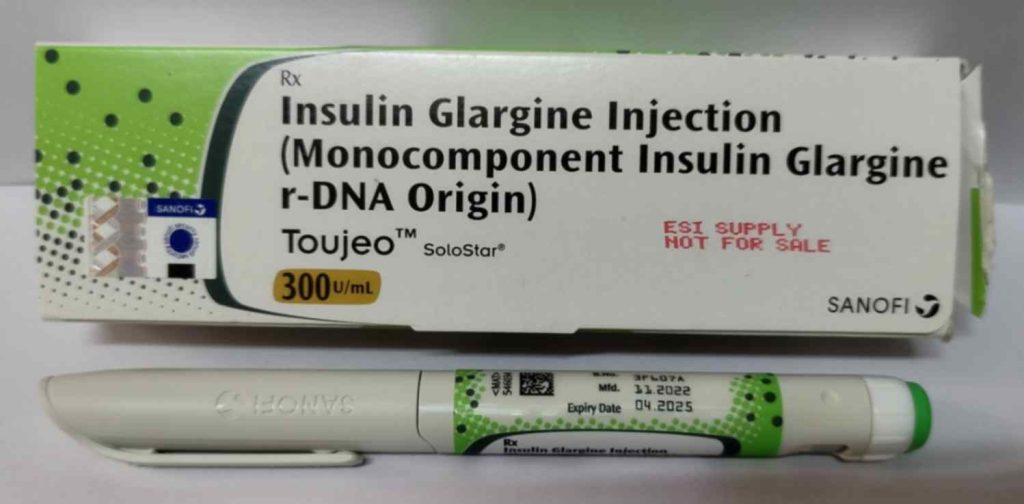
4. Long-acting insulin
It is a long-acting basal insulin analogue. Example of long-acting Insulin is Insulin Detemir and Insulin Glargine.
Insulin glargine is very popular with the brand names Lantus and Basalog, and insulin detemir is available in the Levemir brand name.
These long-acting insulin injections maintain your blood sugar level throughout the night. These injections start to work after 2 hrs.
The duration of action is 24 hrs. It can be injected at any time, but you should take it at the same time every day.
The long-acting Insulin (Lantus) is generally recommended at bedtime.

5. Ultra-long acting insulin
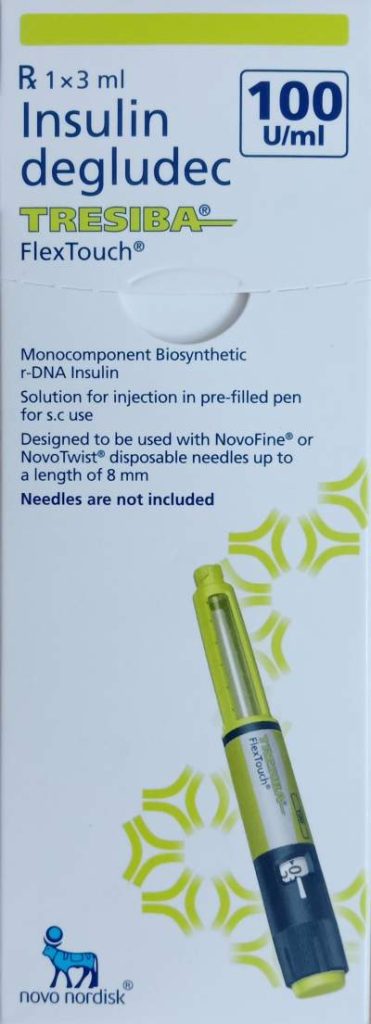
Insulin degludec is an ultra-long-acting basal insulin analogue that prevents strong fluctuation of blood sugar levels. It is very popular with the brand name of Tresiba.
The duration of action of Tresiba is more than 24 hrs and lasts up to 42 hours.
You can inject Tresiba subcutaneously once daily at any time of day.
6. Premixed Insulin
Premixed insulin is a combination of two different types of insulin. It is a fixed composition of rapid or short-acting and intermediate- or long-acting insulin.
Intermediate-acting insulin is commonly used with ultra-short and short-acting insulin to prepare premixed insulin.
This is a combination of bolus and basal insulin analogue.
Premixed insulin formulations are selected according to patient characteristics and based on glycemic patterns to manage diabetes mellitus.
These premixed insulin injections can be injected once, twice or thrice as per patient requirement.
Premixed insulin is available in different combinations –
Combination of intermediate and ultra-short-acting insulin
Despite using intermediate insulin, they have a quicker onset of action. So, you need to inject these injections before 15 15-minute meal.
The examples are –
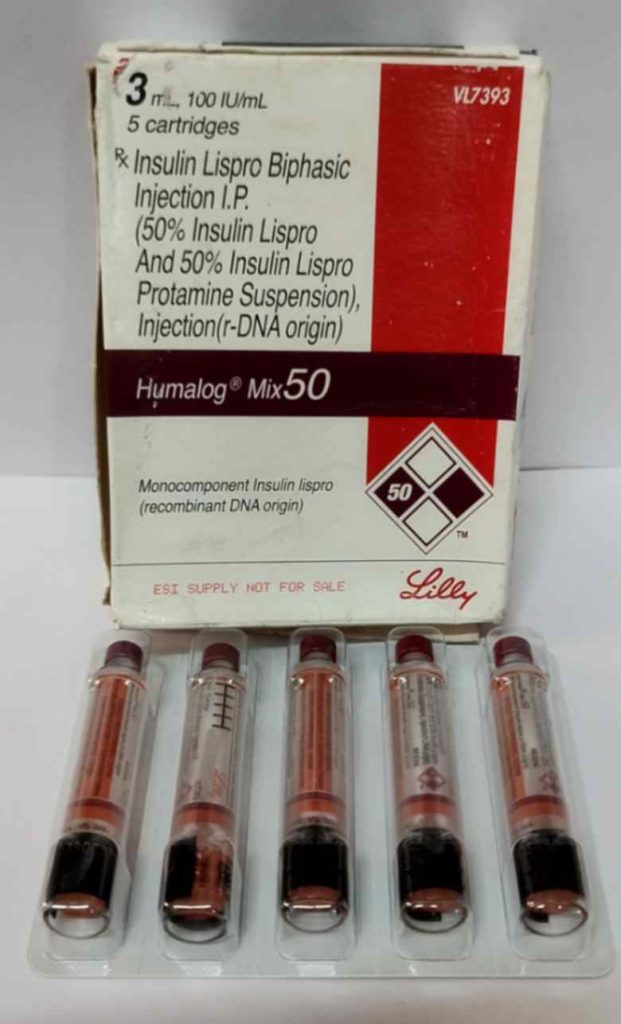
- Humalog Mix 25 (Insulin Lispro 25% + Insulin Lispro Protamine 75%)
- Humalog Mix 50 (Insulin Lispro 50% + Insulin Lispro Protamine 50%)
- NovoMix 30 (30% insulin aspart and 70% insulin aspart protamine)


Combination of intermediate and short-acting insulin
You can see this biphasic human insulin in –
- Wosulin (30% soluble insulin and 70% isophane insulin)
- Human Mixtard 70/30 (70% Insulin Isophane/NPH 70% + 30% Human Insulin/Soluble Insulin)
Here, soluble/NPH insulin is short-acting, and Isophane is intermediate.
It would be best to take this injection 30 minutes before the meal.
Combination of ultra-short and ultra-long-acting insulin
Ryzodec is a classic example of this combination. It significantly controls both fasting and post-prandial blood sugar levels.
Ryzodec contains 70% insulin degludec and 30% insulin aspart.
Here, Insulin degludec is ultra-long-acting insulin. While Insulin aspart is an ultra-short-acting insulin.
It is given once a day immediately before a meal.
What is the role of liraglutide and exenatide in diabetes mellitus?
Liraglutide and exenatide are incretins-based drugs. They are also known as newer antidiabetic drugs. They were introduced in 2005.
These incretin-based drugs are also the last step medication option to control high blood sugar levels.
Although, the mechanism of incretin-based drugs seems to be DPP-4 inhibitors.
But there are some differences in mechanism. DPP-4 inhibitors are incretin enhancers. They indirectly release incretins by inhibiting the DPP-4 enzyme and letting the incretin go to the pancreas.
On the contrary, liraglutide and exenatide are synthetic incretins such as GLP-1 (Glucagon-like peptide-1). These drugs are also called GLP-1 agonists.
These GLP -1 agonist drugs directly release insulin to pancreatic beta cells.
GLP -1 agonist drugs are available in the market in injection form in brands of
- Liruglutide – Victoza and Saxenda injection
- Exenatide – Byetta injection
It can be used in combination with oral triple therapy.
- Metformin + Sulfonylurea + GLP-1 agonist
- Metformin + SGLT2 inhibitors + GLP1 agonist
- Sulfonylurea + SGLT2 inhibitors + GLP1 agonist
- SGLT2 inhibitors + GLP1 agonist
DPP4 inhibitors and GLP1 agonist combinations are not recommended in T2DM due to a similar mechanism.
What is the pharmacological management of diabetes mellitus?
There is a proper way or rules to manage any disease. This treatment plan is called algorithm.
Here, we will know the algorithm for managing T1DM and T2DM.
If you have newly detected diabetes, then the treatment plan should be started in the following ways –
Management of T1DM (Type 1 Diabetes Mellitus)
If a patient has T1DM, there would be few options. It should be started with diet control, exercise and Insulin injections.
Management of T2DM (Type 2 Diabetes Mellitus)
If you have T2DM and your blood sugar level is not controlled by diet modification and exercise.
STEP 1 – Mono-therapy
The primary goal of mono-therapy is to HbA1c <7.5%.
Metformin is an initial therapy (or First-line drug) for treating T2DM. You should be on –
Diet control + exercise + Metformin tablet
If Metformin is contraindicated or intolerant. In that case, the following drugs should be added –
- Sulphonylureas
- Or DPP4 inhibitors “gliptins,” e.g. Sitagliptin, linagliptin, etc.
- Or SGLT2 inhibitors “gliflozins,” e.g. dapagliflozin, empagliflozin and canagliflozin
- Or Pioglitazone
STEP 2 – Dual therapy
Your doctor may start dual therapy if HbA1C > 7.5%.
For non-obese patient
- Metformin + Sulfonylurea, or
- Sulfonylurea + Pioglitazone (If metformin is contraindicated or intolerant)
For obese patient
- Metformin + DPP4 inhibitors or SGLT2 inhibitors or Pioglitazone
If Metformin is contraindicated or intolerant. In that case, the following drugs should be added –
- Sulfonylurea + DDP4 inhibitors
- Or Sulfonylurea + Pioglitazone
- Or DPP4 inhibitors + Pioglitazone
- Or SGLT2 inhibitors + Sulphonylureas
STEP 3 – Triple Therapy
You may require triple therapy if HbA1C > 9%. It can be started in combination with metformin and other antidiabetic drugs –
- Metformin + Sulfonylurea + SGLT2 inhibitors
- Or, Metformin + Sulfonylurea + DPP4 inhibitors
- Or, Metformin + Sulfonylurea + Pioglitazone
- Or, Metformin + Pioglitazone + SGLT2 inhibitors
If metformin is intolerant or Contraindicated, then the patient will require injectable therapy (Step 4)
STEP 4 – Injectable with combinations
There are three options in combination; it can be started as per your need and based on glycemic pattern –
Option 1 – Oral Triple therapy with GLP1
- Metformin + Sulfonylurea + GLP-1
- Metformin + SGLT2 inhibitors + GLP1
- Sulfonylurea + SGLT2 inhibitors + GLP1
- SGLT2 inhibitors + GLP1
Note – Do not use DPP4 and GLP1 in combination.
Option 2 – Oral Triple Therapy with Insulin
- Metformin + Sulfonylurea + Insulin
- Metformin + SGLT2 inhibitors + Insulin
- Metformin + DPP4 inhibitors + Insulin
- Sulfonylurea + DPP4 inhibitors + Insulin
- Sulfonylurea + SGLT2 inhibitors + Insulin
- SGLT2i + DPP4 inhibitors + Insulin
- SGLT2i + Insulin
Option 3 – GLP1 and Insulin
Conclusion
Life does not end with diabetes; it can be managed by lifestyle modification.
The best way to manage diabetes is to educate the patient. Patients should be aware of their diet and exercise. They should know what antidiabetic medicines have been prescribed.
There are proper steps (or algorithms) of antidiabetic medicines to manage diabetes mellitus.
A good doctor always follows the algorithm for the treatment of diabetes mellitus.
This post has discussed the antidiabetic drug classification, mechanism, uses, dosage, and side effects.
These antidiabetic medicines play a significant role in controlling your blood sugar level.
If you found this post informative, please share it on social media.
References –
- D. Tripathi, Essentials of medical pharmacology, 7th Edition. Jaypee Brothers Medical Publishers (P) Ltd; 2013. Chapter – 19, Insulin, oral hypoglycemic agents and glucagon, Page – 258.
- Diabetes education online, university of California. https://dtc.ucsf.edu/
- Electronic medicines compendium (EMC) https://www.medicines.org.uk/emc
- National clinical guidelines for management of diabetes mellitus, 2010, first edition.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2995498/
- https://www.medicines.org.uk/emc/product/594/smpc
- https://dtc.ucsf.edu/types-of-diabetes/type2/treatment-of-type-2-diabetes/medications-and-therapies/type-2-non-insulin-therapies/insulin-sensitizers/
- https://pubmed.ncbi.nlm.nih.gov/11921433/
FAQ
Q 1. What is the first drug of choice for diabetes?
Metformin is the first drug of choice for type 2 diabetes mellitus (T2DM). This medicine should be started initially in newly detected diabetes patients.
Q 2. Which antidiabetic drug class lead to glycosuria?
The SGLT2 inhibitors (dapagliflozin, empagliflozin and canagliflozin) have a unique mechanism to excrete glucose from urine. Due to this, you may have a glycosuria effect.
Q 3. What is the new drug for diabetes?
GLP agonists (Liraglutide and exenatide), DPP4 inhibitors (gliptins), and SGLT2 inhibitors (Gliflozins) are considered newer drugs for diabetes mellitus. Still, the FDA approved Baxagliflozin (SGLT2 inhibitors) on Jan 23, 2023.
Q 4. Is repaglinide safe for kidneys?
Yes. Repaglinide is an absolutely safe and well-tolerated drug in kidney disease patients with type 2 diabetes mellitus.
Q 5. Is linagliptin safe for kidneys?
Linagliptin is mainly (90%) excreted via faeces by hepatobiliary route. It is excreted in small quantities (1 to 6%) through urine. So, Linagliptin (Trajenta) is safe for kidney disease patients.


Arnulfo Pesner
Hello , i just want to share with you this money making method by using CPA ,learn more here >> https://warriorplus.com/o2/a/ps5v5/0
https://warriorplus.com/o2/a/dzkw6/0
Ismael Ruple
Hello , i see the your website get very good daily traffic , why donot you make more money by joining >> https://cutt.ly/ads-wordpress , your daily earning will be increased alongside with adsence try it now for few days and see your daily earning >> https://cutt.ly/ads-wordpress
https://cutt.ly/ads-wordpress
Clemente Mathery
Do you know that the speed of your wordpress website effect your website ranking in google ? you need to check your website speed and chooss the best wordpress hosting company >>https://www.best-wordpress-hostings.org
https://www.best-wordpress-hostings.org/
Janell
Heya this is kind of of off topic but I was wanting to know if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding knowledge so I wanted to get guidance from someone with experience.
Any help would be enormously appreciated!
Feel free to surf to my web page – web hosting companies
Alissa
Very good post. I absolutely love this site. Thanks!
Also visit my webpage; best web hosting 2020
Aurelio
I am actually glad to glance at this webpage posts which carries plenty of
useful data, thanks for providing these kinds of
data. adreamoftrains best web hosting company web hosting
sites
https://www.vfv79.com/
There is clearly a lot to know about this. I consider you made various good points in features also.
카지노사이트
SUMIT SHARMA
Thanks
zortilonrel
Having read this I thought it was very informative. I appreciate you taking the time and effort to put this article together. I once again find myself spending way to much time both reading and commenting. But so what, it was still worth it!
http://www.zortilonrel.com/
Shelton Dickison
thanks for sharing
https://www.ants-medical.com